The Link Between Pets, People and Antimicrobial Resistance

It’s a silly sentiment that reflects a simple fact: we love our pets. If one were to ask the 86.9 million pet-owning households in the U.S. if their companion animals are considered members of the family, the answer would be a resounding, “Yes!”
But people share more than love with their pets. They also share microbes, including antimicrobial resistant (AMR) organisms. Through interactions with their environments and humans, companion animals (e.g., dogs and cats) are emerging as important sources and sinks of AMR microbes—with an emphasis on “emerging.”
“There is a big question mark right now about pets and how they play a role in the spread of [AMR] organisms,” said Cole, who will be moderating a session on the topic at ASM Microbe 2025. “How can we break the chain of transmission if we don't know how pets are involved?”
It’s a good question that has spurred investigations into the dissemination of AMR between people and their animal friends. Such knowledge can ultimately inform the development and deployment of strategies to minimize the risk AMR poses to pets and pet owners alike.
The Rise of AMR in Companion Animals
Researchers have known that pets harbor AMR organisms, particularly bacteria, for a while. However, the prevalence of AMR in companion animals is harder to pin down. While mapping the spread of AMR in people is challenging, the National Antimicrobial Resistance Monitoring System and other surveillance tools help bring the picture into focus. Broadly speaking, fairly limited systems exist for pets, making the picture especially fuzzy (China is an exception, having established the China Antimicrobial Resistance Surveillance Network for Pets in 2021).
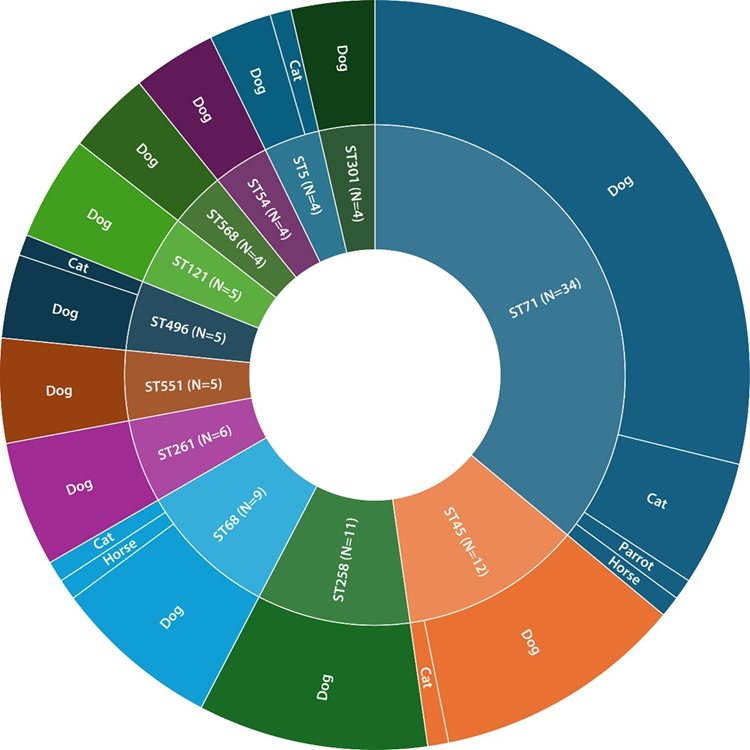
Still, a growing repertoire of research offers some insights. One study found that out of 940 bacterial isolates from infections in companion animals, including species that cause human infections, like Enterococcus faecium, Klebsiella pneumoniae and Pseudomonas aeruginosa, nearly 80% were resistant to at least 1 antibiotic; almost 45% were considered multidrug resistant. Although rates of resistance vary between studies, AMR in pets appears to be common, and the prevalence is likely increasing.What is driving the spread? The reasons mirror those perpetuating AMR in humans. For example, just like health care centers are hotbeds of AMR infections in people, veterinary clinics are environments where resistant organisms survive and thrive, transmitting to and between pets. The more veterinary care a pet requires, the higher the risk of transmission.
Lack of awareness and clarity on antimicrobial stewardship is also part of the problem. When antimicrobials are used indiscriminately, microbes have more opportunities to develop resistance to the drugs. Cole noted that while there are guidelines for antimicrobial use in companion animals, “it primarily [depends] on the goodwill of veterinarians to practice good use of antibiotics,” he said. Pet owners must also comply with prescribed administration, making sure to give the right dose of antibiotic at the right time for the right length of time. How closely veterinarians and pet owners are following antimicrobial stewardship guidelines is a bit of a black box, making it difficult to discern how the drugs are being administered and the potential impact on AMR.
People Spread AMR Microbes to Their Pets—And Vice Versa
This raises a key point: to study AMR in companion animals, one must examine and account for the presence and behavior of the humans who care for them. AMR is, after all, a One Health issue, propelled not just by animals, people and the environment, but also the web of interactions between them. Given that most of the antibiotics used to treat pets are the same as those used in humans, and that many of the same microbes can infect both pets and people, the state of AMR in animals has a direct implication for human health, and vice versa.“We certainly don't think it's a 1-way direction of pets spreading antibiotic resistance to people,” Cole said. “Actually, it probably happens more that people spread it to their pets.” If humans harbor an AMR organism, they can transmit it to their pets directly and indirectly by way of petting, kissing and simply sharing a household environment. Pets can, in turn, transmit AMR microbes to humans and/or other animals. For example, companion animals infected with methicillin-resistant Staphylococcus aureus (MRSA) likely picked up the microbe from humans. On the other hand, dog owners infected by methicillin-resistant Staphylococcus pseudintermedius presumably contracted the bacterium from their pet, as S. pseudintermedius is common in dogs.
Regardless of the source of transmission, microbes can be-bop back and forth between a pet, their owner and other animals/people with whom they engage. The same dynamics apply to AMR genes, which can transmit between bacteria from different hosts. Humans are especially important in facilitating spread, given their social circles and the environments they frequent are larger and more varied than pets.
How often does microbial transmission between pets and people lead to full-blown infection? Cole emphasized that just because a resistant microbe is present doesn’t automatically spell doom for the host. What’s tricky about AMR is that it hinges on potential—an organism could cause problems, but it doesn’t mean it will. The circumstances must be right for AMR to rear its ugly head (e.g., a resistant microbe may live harmlessly in the gut of a cat but trigger a difficult-to-treat infection in their immunocompromised owner). The risk posed by AMR in pets and their humans is, thus, highly individualized, depending on factors like frequency of the medical care and immune status of pets and their owners.
“There are [over] 134 million pets in the U.S., so we're talking about a large population of [animals] that span the gamut of potential risk, and they live very closely with people who also span that gamut,” Cole explained. Understanding human-pet AMR transmission can help researchers frame and mitigate those health risks on a broad scale.
Studying AMR in People and Pets: Techniques and Challenges
To gather this knowledge, scientists use a combination of methods that characterize the presence and movement of AMR organisms in and between pets and humans, leveraging everything from antimicrobial susceptibility testing to genomics.
There are challenges to compiling these data, however. For one, many studies do not examine isolates from both animals and their human companions when conducting susceptibility testing and strain typing. Yet, this is critical for piecing together the puzzle of AMR transmission in humans and pets. Moreover, Cole noted that electronic medical record keeping is still evolving in veterinary medicine, with a lot of different approaches used. Electronic medical records (EMRs) contain loads of health information that can be mined for studies into the characteristics and trends of diseases and issues like AMR infections. The complexity of medical record keeping in veterinary medicine means epidemiological investigations in pets is a lot trickier.
There is also a cost component. Pet care is not typically covered by insurance, so “doing antimicrobial susceptibility testing is a cost that goes directly to the owners,” Cole said. Many owners will opt out of these tests because completing them is not economically desirable or feasible. “There is a lack of data because of a lack of support to do this kind of work in animals.”
ASM is expanding its portfolio of journals with the launch of ASM Animal Microbiology, a journal dedicated to advancing research on animal-associated microbes and their impact on health, disease and productivity. To lead this new journal, ASM Journals is looking or an editor in chief to begin a 5-year renewable term on July 1, 2025. Interested?
The Way Forward
The moral of the story is that we need more information—and the resources to collect it. There is plenty of evidence pointing to the presence of AMR microbes in pets, and their bidirectional exchange with people, but most of it comes from case studies or smaller prevalence studies. More extensive, longitudinal analyses are required to fully grasp the magnitude and breadth of the problem.For Cole, the future of the field depends on collaboration between public health departments and veterinary practices. “I would love to see more collaboration across the sectors. How do we manage data across the veterinary industry and tie that together with the human side? It’s a complicated question, but an important question as well.” Someday, pet data could become a key component of AMR surveillance systems, providing a clearer picture of how resistant microbes spread within our communities. This could influence both veterinary and medical approaches to treating AMR infections. Regularly collecting data on pets and pet owners in health care and veterinary settings would help determine an individual’s risk of AMR exposure or help pinpoint the source of an infection.
Caring for Pets With AMR in Mind

At home, owners can do their part by keeping animals and homes clean, washing their hands after playing with or snuggling with their pets and minimizing intimate contact, like face licking (in which the pet licks their owner’s face, though it is probably best if owners avoid licking their pet’s face, too).
Cole acknowledged that the relationship people have with their pets is special and multi-faceted. The goal is to preserve that relationship with AMR in mind. “I look at this as not only a project of protecting human health and animal health, but also that bond that exists between people and animals too, because we know pets add a huge amount of value to our lives. That's why investigating this is so important, because we intersect with them so often.”
Whether your research deals with AMR or any number of other topics spanning the microbial sciences, join us at ASM Microbe to learn about cutting-edge research your field.

